What is thyroid eye disease and can it be treated?
Thyroid eye disease is an autoimmune eye condition that is often seen in people with thyroid disease and is usually abbreviated TED. It tends to run in families and is more frequent in women and in smokers. When you have TED, your immune system mistakenly attacks the muscle and fat tissue behind your eyes, causing inflammation, redness, and swelling as well as causing scar tissue to form.
More severe effects from TED are rare, but can occur, including vision loss from damage to the optic nerve and breakdown/infection of the cornea (the transparent, outermost layer of the eye). About 90% of TED patients also have Graves’ Disease. However, about 10% of TED patients have a normal or under-functioning thyroid.
TED can be seen in conjunction with Graves’ Disease, Grave’s ophthalmopathy or orbitopathy (GO), or Thyroid-associated orbitopathy (TAO). About 30% of people with Graves’ Disease have a mild form of thyroid eye disease while 5% develop a severe form. The condition is also seen in people with no evidence of thyroid dysfunction or in people diagnosed with Hashimoto’s disease, a hypothyroid autoimmune condition marked by an underproduction of thyroid hormones.
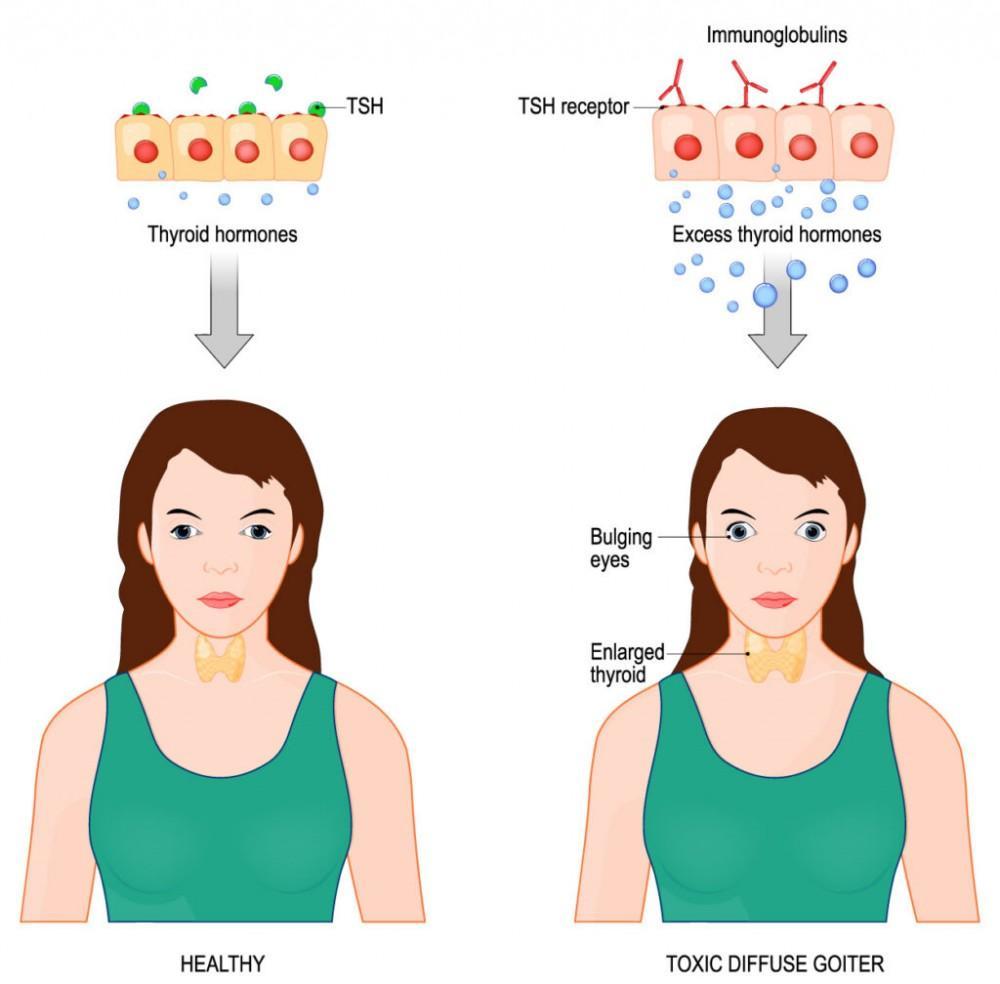
Graves’ Disease, also known as toxic diffuse goiter, is an autoimmune disorder that results in the overproduction of thyroid hormones (hyperthyroidism or an overactive thyroid). Graves’ is the most common cause of hyperthyroidism and usually results in an enlarged thyroid. When the thyroid gland is overactive, the body’s processes speed up. This “speeding up” may cause irritability, muscle weakness, sleeping problems, a fast heartbeat, poor tolerance for heat, diarrhea, unintentional weight loss, nervousness, anxiety, hand tremors, excessive sweating, and hair loss, among other symptoms. Some individuals even experience problems with memory, focus, and depression.
Graves’ ophthalmopathy or orbitopathy (GO) is a thyroid eye disease that can affect both a person’s vision and their physical characteristics.
Thyroid-associated orbitopathy (TAO) is an inflammation behind the eye that affects fat and extra-ocular muscles that causes the eye to protrude. The upper eyelids also are involved as they pull back, adding to the appearance of excessive protrusion. It can create dryness, burning, and eye irritation. TAO affects women more frequently than men between the ages of 40 and 60.

What are the symptoms of thyroid eye disease? Does it hurt?
Symptoms appear suddenly and often worsen quickly. The inflammation and scarring that occurs can damage your eyes. It’s important to see a specialist right away to begin treatment. The pain associated with TED relates to the symptoms which can be treated to prevent persistent pain and emotional distress. Symptoms may include some or all of the following:
- Movement of the eyeball up, down, or sideways causes pain
- Difficulty in moving the eyes up, down, or sideways
- Inflammation and swelling of the eye causing eye to push forward giving the appearance of bulging (exophthalmos)
- Dryness, itching, burning and irritability of the eyes
- Excessive tearing
- Double Vision
- Appearance of redness or bloodshot eyes
- Light sensitivity
- Impaired vision or double vision (diplopia)
- Optic neuropathy
- Eyes not in alignment with each other
- Feelings of anxiety and depression, loss of confidence
Can thyroid eye disease go away?
Thyroid eye disease is known to go into periods of remission and can have varying degrees of severity. It sometimes is active for six months to three years. If it is inactive for six months, it usually remains inactive, but that doesn’t mean it goes away. You may still have mild symptoms that if left untreated, it can flare up again.
TED has two phases. The acute phase which means the disease is active and the chronic phase which is the inactive or stable period of thyroid eye disease, a period when it slows down with few or no symptoms.
Can thyroid eye disease affect only one eye?
It may affect only one eye, or one eye more than the other. Thyroid eye disease may begin with either one eye or both or one eye may have more severe symptoms. It is not known why this can occur.
Does everyone with Graves’ Disease get bulging eyes?
The people that are diagnosed with Graves’ ophthalmopathy have a condition wherein inflammation and other autoimmune activity affects muscles and other tissues around the eyes, which may result in the appearance of bulging eyes (exophthalmos). Only about 30% of people with Graves’ Disease develop exophthalmos.

Does Graves’ Disease get worse over time?
Graves’ Disease, if not treated, can over time cause heart damage and erratic behavior due to negative effects on the brain. When the thyroid gland is overactive, the body’s processes speed up. This “speeding up” may cause irritability, muscle weakness, sleeping problems, a fast heartbeat, poor tolerance for heat, diarrhea, unintentional weight loss, nervousness, anxiety, hand tremors, excessive sweating, and hair loss, among other symptoms. Some individuals even experience problems with memory, focus, and depression.
How quickly does thyroid eye disease progress?
There are two phases of Thyroid Eye Disease. The first phase is called the acute phase, or active phase when symptoms are apparent. The second is called the chronic phase, or the inactive phase when there are few or no symptoms.
Thyroid Eye Disease begins with the acute phase, when symptoms appear suddenly and usually worsen quickly. Redness and swelling (inflammation) and scarring start to form during this phase and can damage your eyes and cause a number of other changes. As soon as you notice any symptoms, contact your specialist to schedule a thorough eye exam before any eye damage can be done.
Would you like to talk with someone about your vision? Contact us today at (843) 553-2477 to schedule an appointment.
Can you drive with thyroid eye disease?

In the early stages before damage is done, a patient should have no trouble driving. However, there are some symptoms of hyperthyroidism that would prevent you from seeing properly when driving.
- Advanced symptoms may cause a physician to advise against driving while symptoms persist. The physician will review and report on the patient’s visual capacity regularly and oversee possible side effects of medications prescribed.
- A patient would not be able to drive with symptoms that reduce the psychophysical capacity.
- Thyroid crisis or storm would prevent a patient from driving until the problem is solved.
- After thyroidectomy surgery, the patient cannot drive for three weeks and can drive only after the surgeon’s assessment of the clinical recovery of the patient.
What is the best treatment for thyroid eye disease?
From an ophthalmologist’s perspective, the primary goal of treatment is to prevent loss of visual function, while at the same time, taking steps to prevent other disfunctions of the eye that can occur. Treatment becomes less effective as the disease progresses from the early, acute phase to the chronic phase. In fact, treatment initiated during the early months of the active phase has been shown to be most effective; whereas, treatment that is begun during the late stages of the active phase, has shown to have little effect on the final outcome of disease. Once the chronic stage has set in, treatment options become more limited and is primarily surgical.
About seventy-five percent of patients with thyroid eye disease (TED) have mild to moderate symptoms and require primarily symptom management, such as eye lubrication (daytime eyedrops and nighttime ophthalmic ointment). Sometimes topical cyclosporine is prescribed to reduce symptoms of ocular surface irritation. Lifestyle changes are also helpful, such as smoking cessation, as smoking cessation helps prevent further development of the disease and decreases the duration of the active phase. Sodium restriction (salt) to reduce water retention and edema in the eye tissue is beneficial as well as sleeping with the head elevated to decrease orbital edema.

Medical treatments include Oral steroids, ILGF-1 monoclonal antibody infusions (Tepezza®), and/or orbital radiation. Talking with your doctor can help to decide if any of any of these treatments are right for you.
About twenty percent of patients with thyroid eye disease undergo some type of surgical procedure such as eyelid surgery, strabismus surgery and orbital decompression surgery. Generally, surgery is not advised until the TED has been in the stable phase for at least 6-9 months with the exception being visual loss from compressive optic neuropathy or corneal exposure, which both require urgent surgical intervention.
TED can also be disfiguring and can be emotionally and psychologically challenging for many patients. The symptoms that come and go can be wearisome for all concerned. It’s important to get involved with one of the Peer Support Groups that are available in order to stay hopeful and encouraged.
Do ophthalmologists treat thyroid eye disease?
Yes, some ophthalmologists treat thyroid eye disease. TED Specialists have special training in one area of ophthalmology, such as surgical procedures. The following are the types of specialized ophthalmologists that you could see.
- Oculoplastic surgeons
- Neuro-ophthalmologists
- Strabismus specialists/surgeons
- Retina/Vitreous specialists
- Cornea specialists
Contact us at (843) 553–2477 to speak with a specialist that can find the answers you need.
What is the thyroid gland?

The thyroid gland is situated in the front portion of the neck and is shaped like a butterfly, covering the windpipe from three sides. It secretes two hormones, Triiodothyronine (T3) hormone and the Thyroxine hormone (T4). These hormones regulate the metabolism of the body and therefore affect almost every tissue in the body.
How is thyroid eye disease diagnosed?
To diagnose thyroid eye disease, you will need a complete eye exam, lab tests, and imaging tests. The ophthalmologist will test your vision, color vision, and visual fields. In addition, eyelid measurements will be taken, eye pressure tested, and optic nerve checked. An exophthalmometer will be used to measure the degree (if any) of eye bulging and if and how far forward your eyes have moved due to TED.

If you have not already had a diagnosis of Graves’ Disease, the doctor may order laboratory tests to confirm whether you do or not have Graves’. However, you may not need these tests if you already know that you have Graves’ Disease.
You will need blood tests to check the levels of thyroid-stimulating hormone (TSH), Thyroxine (T4), Triiodothyronine (T3), Thyroid-stimulating immunoglobulin (TSI), Thyroid-stimulating hormone receptor antibody (TRAb), and anti-thyroid peroxidase antibody (anti-TPO).
If you do not have a previous diagnosis of Graves’ Disease, you may have the following imaging tests:

- Radioactive iodine uptake test with X-rays to check how the thyroid collects iodine
- Ultrasound of the thyroid to see if it is enlarged or has nodules
- CT scan to check for an enlarged thyroid and nodules
- MRI to check for an enlarged thyroid and nodules
If you already know that you have Graves’ disease, a CT scan and MRI will be taken to check the condition of your eyes and eye muscles. These imaging tests can show inflamed tissues, enlarged muscles, and compressed optic nerves in the eyes.

There is a possibility for some symptoms of TED to be similar to other conditions, such as orbital tumors. Your ophthalmologist will be treating the TED (Thyroid Eye Disease) specifically, while working closely with your primary care physicians/endocrinologists, who will be the ones managing/monitoring the Thyroid disease. Your doctor will do testing to confirm your condition. When looking at the whole picture: the results of a physical exam, lab tests, and imaging tests, it can be determined whether you have thyroid eye disease or something else.
Contact us at (843) 553–2477 to speak with a specialist that can find the answers you need.

